Have you ever wanted to see a doctor that isn’t in-network? What exactly does that mean? And how important is it to only see providers who are in-network?
What Is a Health Insurance Provider Network?
In-Network: Health insurance companies contract with doctor’s offices and hospitals to pay lower prices for their services, in return for more patient traffic. The provider agrees to accept the lower rate, which includes your copay or coinsurance, as payment in full. These providers – doctors, specialists and hospitals – are considered in-network.
Out-of-Network: If a doctor or hospital is not contracted with your health insurance plan then they are out-of-network. This means there is no discount applied to the service you receive from that provider and you may be charged a much higher rate than if the provider had been in-network. Often, health insurance plans also try to discourage members from going out-of-network by charging them higher copays, coinsurance, and deductibles.
Why Does It Matter?
When you see a network provider, you can feel confident that s/he or the facility has met certain qualifications, such as educational background, safety measures and board certifications, required by your insurance company. This assurance of quality is in addition to the in-network cost savings you will receive by going to your insurance company’s approved providers.
As mentioned above, seeing an in-network provider can result in a substantial cost savings. For example, let’s say you’re visiting a dermatologist to have a cyst removed and you’re covered by a PPO plan. Let’s also assume you’ve met your plan’s deductible for the year. Here’s a comparison of what the charges might look like:
How your plan pays for out-of-network services depends on the type of coverage you have.
HMO & EPO: If your health insurance is provided by a Health Maintenance Organization (HMO) or an Exclusive Provider Organization (EPO) then your plan does not pay for any services with providers that are out-of-network, except in the case of a true medical emergency.
PPO & POS: If your health insurance is provided by a Preferred Provider Organization (PPO) or a Point-of-Services (POS) plan, then your insurance company will likely pay for some of the fees from out-of-network doctors – but you must share more of the costs. For example, the plan may cover 80% of in-network care but only 60% of out-of-network services. And some out-of-network services might not be covered at all.
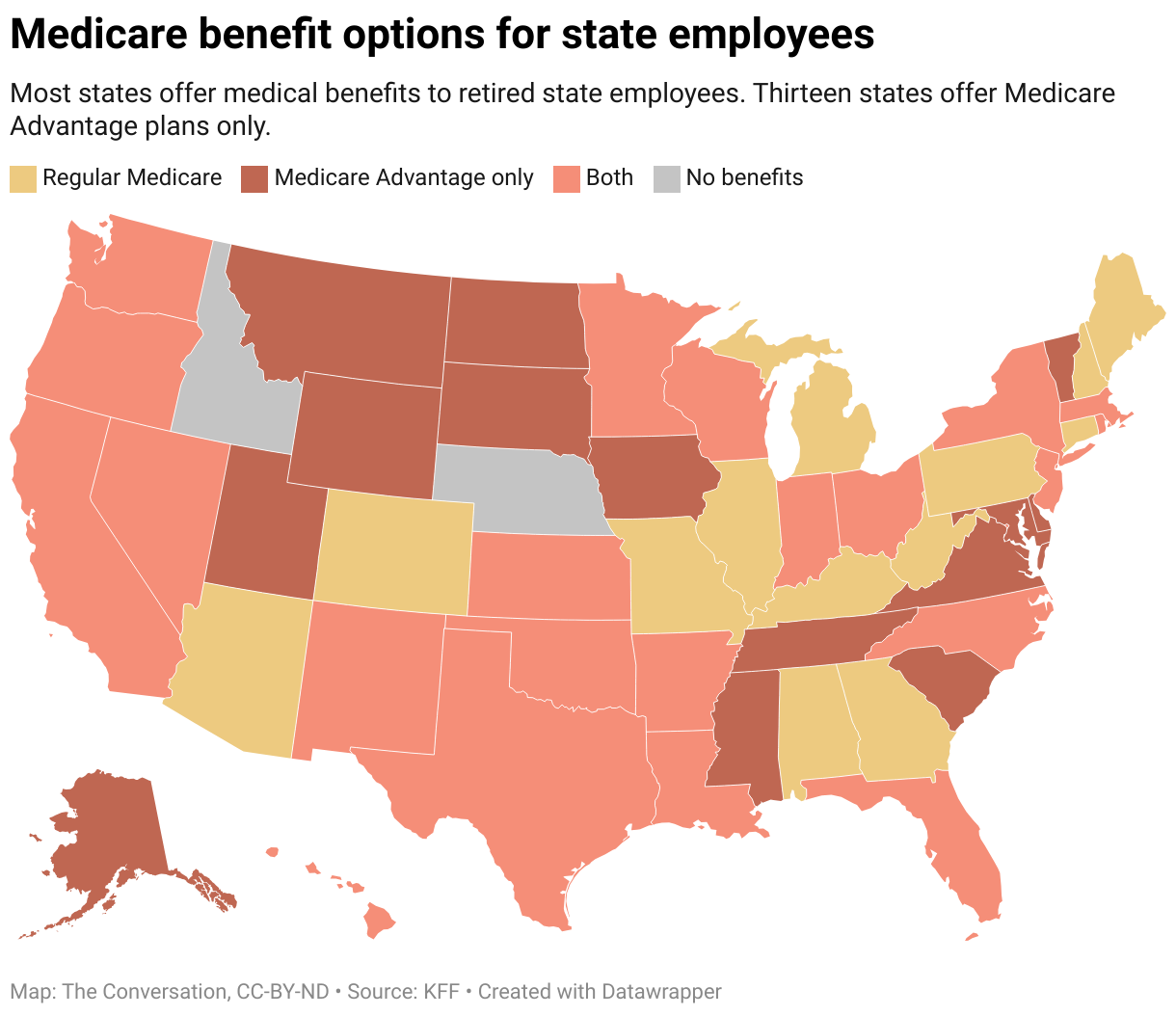
Medicare: If you only use Original Medicare (Medicare Part A & Medicare Part B), or if you use a Medicare Supplement plan, any doctor who accepts Medicare is in your network. If you have Medicare Advantage (Medicare Part C), you have to determine how that particular plan works and whether it has a network you must use for providers. For instance, less common Medicare plans like a Medicare Special Needs Plan may have small, restricted networks.
Remember, even with a Medicare supplemental plan, going to an in-network provider instead of one out-of-network can mean a substantial cost saving for you. In fact, bills from an out-of-network provider may not be covered at all.
How Do You Know Who’s In-Network?
You can find out if a specific provider is in-network for your plan by calling the toll-free number on the back of your medical plan ID card or visiting the plan’s website (most have a “Find a Provider” page). Because providers go in- and out-of-network with some regularity, you should check from time to time to make sure your provider is still in-network.
You can also call the provider directly and ask. Be sure to specify both the insurance company and the specific name of the plan – for example, BlueCross BlueShield of Alabama Blue Care Network. Your provider may have negotiated a contract with one insurance company’s plan but not all of them – so just because they accept your insurance doesn’t necessarily mean they’re in your network.
While staying in-network should be pretty straightforward, there are times when you’ll accidentally find yourself with out-of-network charges.
Accidentally Going Out-of-Network
Have you ever gotten treatment, checking ahead of time that your care will be considered in-network, but later receiving a bill for out-of-network charges? You’re not alone – 7 in 10 people with out-of-network bills didn’t know their provider was out-of-network until they were billed, according to a Kaiser Family Foundation survey.
Scenario 1: Let’s say you’re having surgery. Before agreeing to the procedure, you check that the surgeon and the hospital are in-network to be sure you’re covered. But it turns out the anesthesiologist who assisted your surgeon isn’t in your network. Unfortunately, you’re charged a higher out-of-network rate than if this specialist had been in-network. You can try to negotiate with the anesthesiologist’s billing office but most likely, there won’t be much you can do to lower your bill.
The best way to avoid this is to ask your surgeon (or their team) to make sure all providers are in-network before your surgery – and to get it in writing. If you’ve already seen an out-of-network doctor, you could try to work out an arrangement with the hospital or your health insurance company. Also, if you’re covered by your employer’s plan, check its policy on balance billing, which is explained further down in this article.
Scenario 2: You visit your doctor, and he or she refers you to a specialist, who happens to not be in your plan’s network. Before you visit any new doctor, check to make sure that specialist is in your network. If he or she isn’t, call your primary care doctor back and ask for a referral to a provider within your network. In some cases – for instance if there are no in-network providers in your area – your plan may cover bills from an out-of-network provider. Always try to check with your insurance company before your procedure to determine if a provider will be covered.
When Should You Go Out-of-Network?
While staying within the boundaries of your network sounds tricky, they’re usually set up so that you won’t have to go out-of-network. Doctors of all types and specialties are typically included so you should always be able to get the services you need from inside your own provider network.
That being said, in the rare case when you can’t find an in-network provider, health insurance plans will review the medical necessity of the situation and potentially make an exception or try to contract with the doctor to bring them in-network.
In the case of life-threatening emergencies, you should always go to the nearest emergency room. Insurance should always cover you if you have to see an out-of-network provider in these circumstances. However, there have been cases where patients are charged exorbitant out-of-network fees when they receive a service after they’ve been admitted to the hospital – that is, once they’re moved out of the emergency room – or if it’s determined that the situation wasn’t a true medical emergency. It’s best to refer to your plan’s specific rules regarding this situation.
| What About Centers of Excellence? Some plans negotiate special deals with “Centers of Excellence.” These are institutions that have shown exceptional quality of care and outcomes as well as cost-effectiveness in specific areas. In many cases, your coverage will be dramatically reduced if you don’t make use of this “narrow network” to receive care. Centers of Excellence are usually associated with conditions such as organ transplants, orthopedics, cancer and bariatric surgery, to name a few. |
Out-of-Network Charges and Balance Billing
The Affordable Care Act (Obamacare) prohibits insurance companies from charging higher cost-sharing for out-of-network services in cases of emergencies. However, it doesn’t prevent the hospital from billing patients directly.
“Balance billing” happens when the provider bills you the difference between what the health insurance company paid and what the provider charges. Since the provider is out-of-network and there is no contract with your health insurance company, the provider can go directly to you to recoup their costs.
In the example above, assume the out-of-network doctor normally charges $400 to remove a cyst. Your plan bases its charges on the “reasonable and customary” amount, which is $250. As a result, your plan will cover $125, which is 50% of the $250 reasonable and customary charge. You will be billed for the other $125, plus the doctor can then charge you the difference between his $400 charge and the $250 he received from the insurance company, or $150. This means you will pay a total of $275 for the doctor’s $400 bill.
Some states are trying to provide more protection to patients by restricting providers from balance billing patients. While fully-insured plans are subject to state regulations, several states are trying to go further. For example, New York has created legislation to protect individuals in certain circumstances from being balanced billed. And there are efforts underway to introduce federal protections as well.
In the meantime, you can protect yourself by making every effort to see a network provider, documenting any instance where you might not have had a choice of provider (for example, in the case of an emergency admission), and contacting the provider to see if you can work something out. See “How to Best Prepare Yourself for Negotiating Medical Bills” for additional guidance.